The majority of those who have had their eyes examined will understandably view vision in a rather binary way. Either things are blurry, or you modify your glasses or contact lenses to make things clear – end of story.
For those with issues related to balance, dizziness, reading challenges or light/motion sensitivity, however, this rather succinct summation of vision doesn’t quite cut it. When people view the aesthetic appearance of someone’s glasses, they generally look rather similar. Maybe a scratch here, a reflection there – but it’s often challenging to distinguish the difference between two people’s lenses at a cursory glance. Because of these similarities, and because the general public (and nearly all healthcare practitioners) understand very little about optics, people can often go months, or even years, wearing glasses that are holding them back.
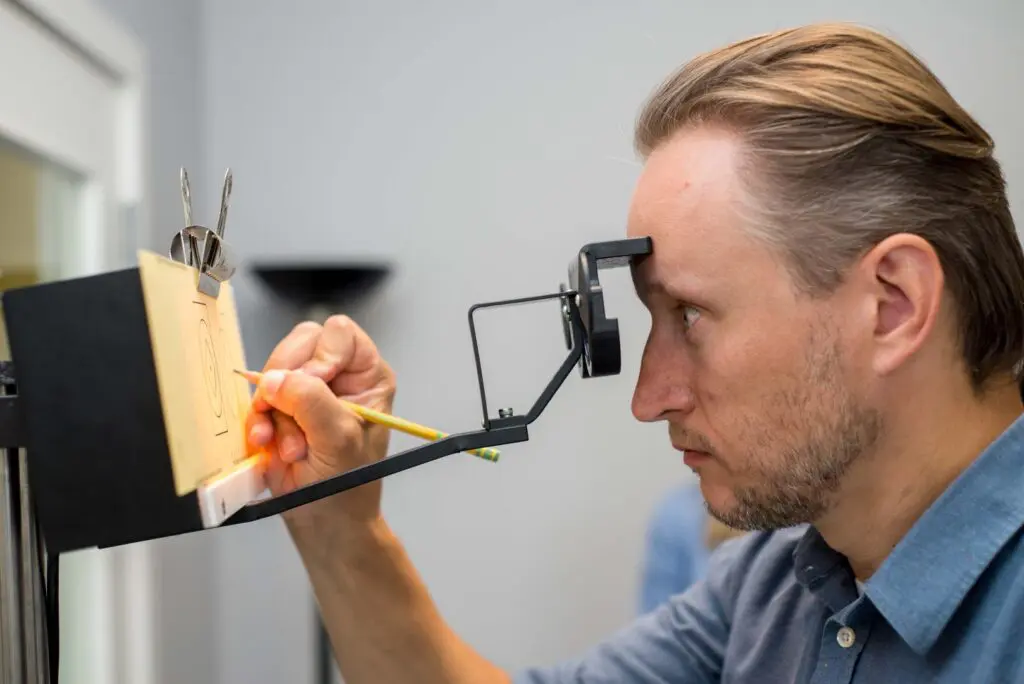
When we think about the components of our visual system that drive balance, orientation and reading skill, it is imperative to understand that our central clarity (ie: 20/20 vision, “what is it” pathway) is far less important than our peripheral vision (“where is it” pathway). Imagine yourself in a traditional eye exam – lights off, sitting down, viewing tiny letters 20 feet away through a pinhole opening. One or two – which is clearer, darker and blacker? While this is of course a relevant measure, ask yourself, what is missing from this process? Peripheral vision!
In order to engage the peripheral visual stream, it is important that portions of your visual assessment are conducted in a manner that allows peripheral awareness – as would occur in the real world. What does this mean exactly? You should be up, moving and assessed in free space – not entirely in a small dark exam room. I tread cautiously with this statement, mind you, as it is still very important to have traditional measures taken – though they need to be combined with and considered alongside assessment of visual skills in more real-world environments.
After a decade of experience providing therapeutic eyeglass prescriptions, I can tell you with certainty that the glasses prescriptions which provide the best sense of balance and orientation, reduced dizziness and improved reading skill are almost never the glasses that provide the best central clarity in an exam room. I do understand that this is a rather bold statement – and might catch people a little off guard. An optometrist might even have a visceral objection to this statement, particularly if they haven’t objectively measured balance or reading fluency using a variety of different lens prescriptions. But, it’s nearly impossible to argue with thousands of cases of direct feedback – these previous lenses make me feel dizzy and uncomfortable reading, while the new ones do not. Practically, what matters most is choosing both a prescription and lens design that allows for reasonable central clarity while also keeping peripheral vision engaged. And a combination of experience, in-office glasses trials and objective measures of balance and reading fluency is what allows one to settle on just the right solution.
If you or a loved one is struggling with dizziness, balance issues, light/motion sensitivity or reading struggles, be sure to ask – were my glasses prescribed and assessed while I was doing the types of things that trigger my symptoms? Did the examiner watch me reading? Was I assessed while viewing a computer or phone? Was I assessed while moving through a busy visual environment? If the answer is no, and you continue to struggle with many of the symptoms discussed and outlined above, I might suggest a second opinion – and a chance to further investigate whether a prescription modification could help further guide you along the path towards recovery.
Until next month,
Paul Rollett, OD, FCOVD